How Hypothalamus Disorders Disrupt Male Hormones and Fertility
Male fertility depends on a finely balanced hormonal system, and at the center of this system lies a small but powerful part of the brain called the hypothalamus. Many men facing unexplained infertility are unaware that the root cause may begin in the brain rather than in the testes themselves. Understanding hypothalamus disorders is essential for early diagnosis, effective treatment, and long-term reproductive health, especially under the guidance of an experienced hormonal specialist, Dr. Abhishek Shrivastava.

Understanding the Role of the Hypothalamus in Male Fertility
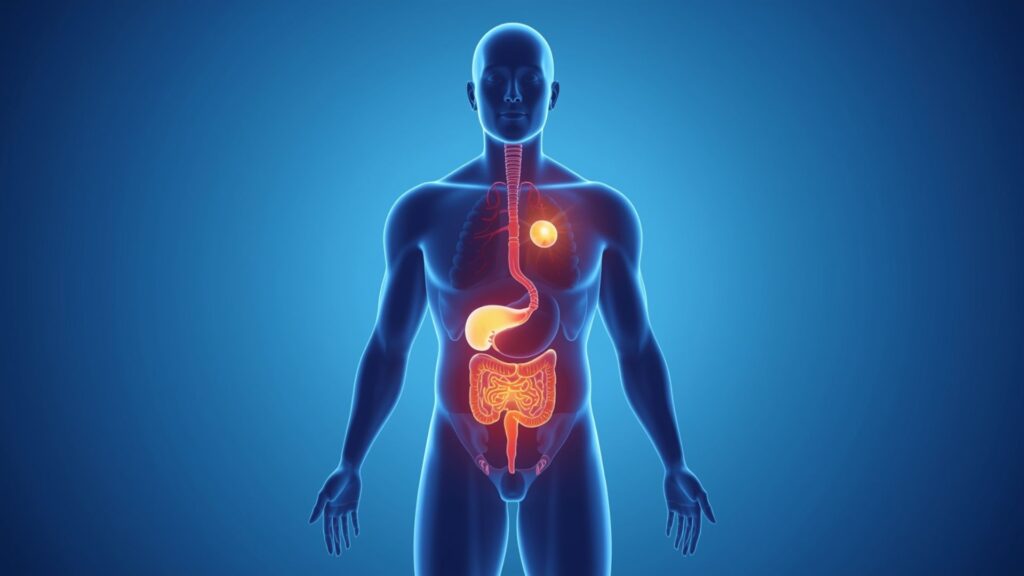
The hypothalamus is a critical control center that links the nervous system with the endocrine (hormonal) system. Its primary role in male fertility is to release Gonadotropin-Releasing Hormone (GnRH) in a pulsatile manner. This hormone signals the pituitary gland to produce two key hormones: Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH).
LH stimulates the testes to produce testosterone, while FSH supports sperm production. When the hypothalamus does not function properly, this hormonal chain is disrupted, leading to low testosterone levels, poor sperm production, or even complete infertility. According to hormonal specialist Dr. Abhishek Shrivastava, many cases labeled as “idiopathic infertility” actually have a hidden hypothalamic origin.
How Hypothalamus Disorders Affect Male Fertility
Hypothalamic disorders can affect male fertility in several ways:
- Reduced GnRH secretion: This leads to low LH and FSH levels, directly impacting sperm count and quality.
- Low testosterone levels: Testosterone is essential for libido, erectile function, and sperm maturation.
- Delayed or absent puberty: In younger males, hypothalamic dysfunction may prevent normal sexual development.
- Poor sperm parameters: Reduced motility, abnormal morphology, or azoospermia (absence of sperm).
Conditions such as Kallmann syndrome, chronic stress, excessive weight loss, obesity, head trauma, tumors, and long-term systemic illness can damage hypothalamic function. Hormonal specialist Dr. Abhishek Shrivastava emphasizes that early identification of these factors can significantly improve fertility outcomes.
Signs and Symptoms That Should Not Be Ignored
Men with hypothalamus-related fertility issues may experience:
- Low sex drive
- Erectile dysfunction
- Fatigue and low energy
- Loss of muscle mass
- Infertility despite normal testicular size
These symptoms are often subtle and gradually progressive, which is why expert evaluation by the best endocrinologist in Jabalpur, Dr. Abhishek Shrivastava, is crucial for accurate diagnosis.

How to Test for Hypothalamus Disorders
Diagnosing hypothalamic disorders requires a step-by-step approach. There is no single test, but a combination of clinical evaluation and investigations helps confirm the diagnosis:
- Hormonal blood tests: Measuring testosterone, LH, FSH, prolactin, and thyroid hormones.
- GnRH stimulation test: Helps assess how the pituitary responds to hypothalamic signals.
- Semen analysis: Evaluates sperm count, motility, and morphology.
- MRI of the brain: Used to detect structural abnormalities, tumors, or injury in the hypothalamic-pituitary region.
- Detailed medical history: Including lifestyle factors, stress levels, weight changes, and past illnesses.
Hormonal specialist Dr. Abhishek Shrivastava often highlights that proper interpretation of these tests is more important than the tests themselves.
Can Hypothalamus-Related Infertility Be Treated?
Yes, in many cases, hypothalamus-related infertility is treatable. Treatment depends on the underlying cause and may include:
- Hormone replacement therapy
- Pulsatile GnRH therapy
- Treatment of underlying conditions, such as obesity or nutritional deficiencies
- Stress management and lifestyle correction
Under the supervision of hormonal specialist Dr. Abhishek Shrivastava, many patients experience restoration of normal hormone levels and improved fertility potential.

How to Prevent Hypothalamic Disorders
While not all hypothalamus disorders can be prevented, certain measures can significantly reduce risk:
- Maintain a healthy body weight
- Avoid extreme dieting or over-exercising
- Manage chronic stress effectively
- Get adequate sleep
- Avoid anabolic steroids and substance abuse
- Seek early medical advice for hormonal symptoms
Preventive care and timely consultation with hormonal specialist Dr. Abhishek Shrivastava can help protect long-term reproductive health.

Common Myths Corrected
A common misconception is that male infertility always originates in the testes. In reality, the brain—especially the hypothalamus—plays a central role. Another myth is that hormonal infertility is permanent; with modern therapies and expert care, many cases are reversible.
Frequently Asked Questions (FAQs)
What is the connection between the hypothalamus and male fertility?
The hypothalamus controls the release of GnRH, which regulates LH and FSH production. These hormones are essential for testosterone production and sperm formation.
How to test for hypothalamus disorders?
Testing involves hormonal blood tests, semen analysis, GnRH stimulation tests, and brain imaging such as MRI.
How to prevent hypothalamus disorders?
Maintaining a balanced lifestyle, managing stress, avoiding substance abuse, and seeking early medical evaluation are key preventive steps.
Can hypothalamus disorders cause low sperm count?
Yes, reduced GnRH secretion can lead to low FSH levels, resulting in poor sperm production.
Is hypothalamic infertility permanent?
Not always. With proper diagnosis and treatment from Jabalpur’s best Endocrinologist, Dr. Abhishek Shrivastava, many men can regain normal fertility.
Conclusion
Hypothalamus disorders are an often-overlooked but highly significant cause of male infertility. Understanding the brain–hormone–fertility connection allows for targeted treatment and better outcomes. With expert care from an endocrinologist in Jabalpur, Dr. Abhishek Shrivastava, men facing fertility challenges can find clarity, effective treatment options, and renewed hope for parenthood.
